Ft. Worth Brain & Spine Institute
A new paperless system for seamless PHI collection and distribution
Legacy System
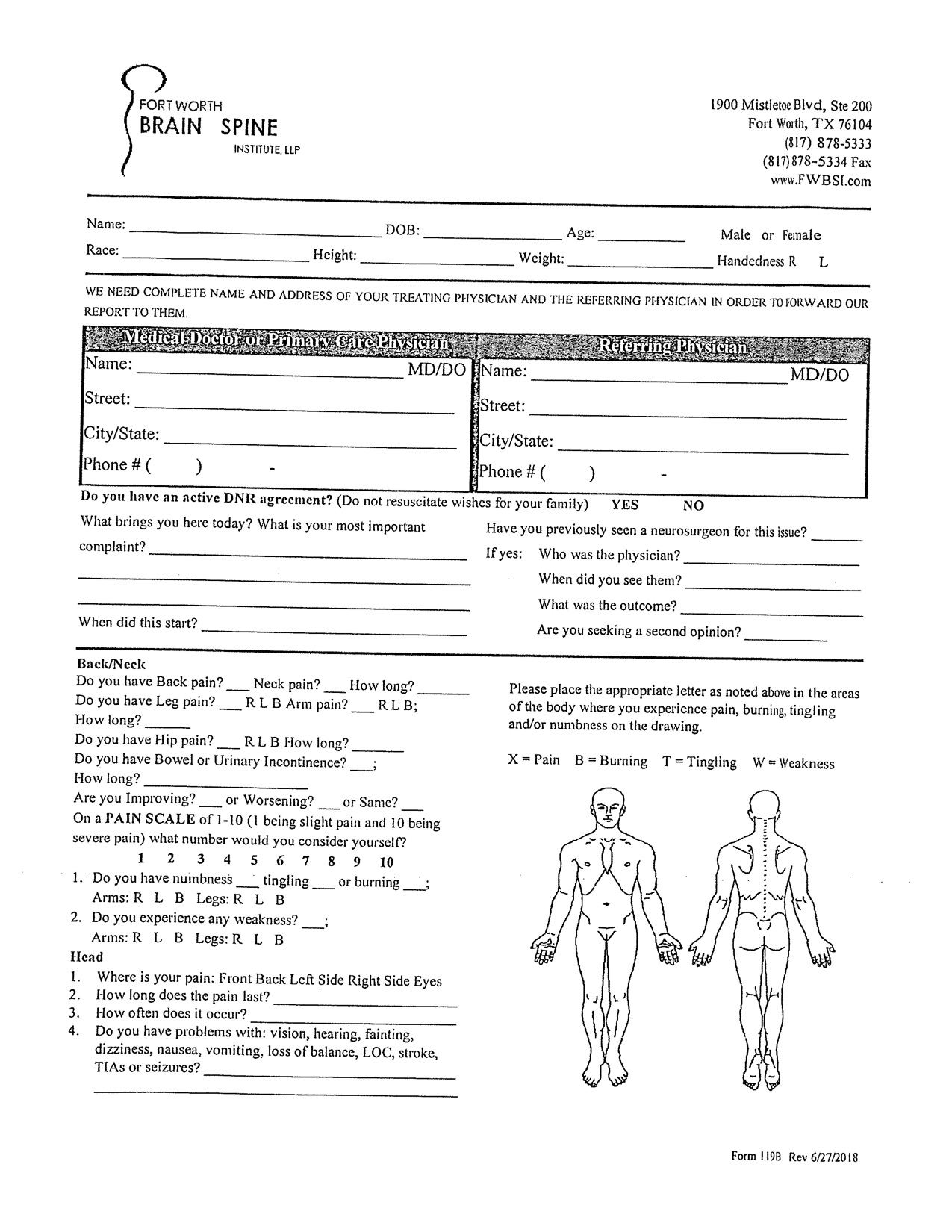
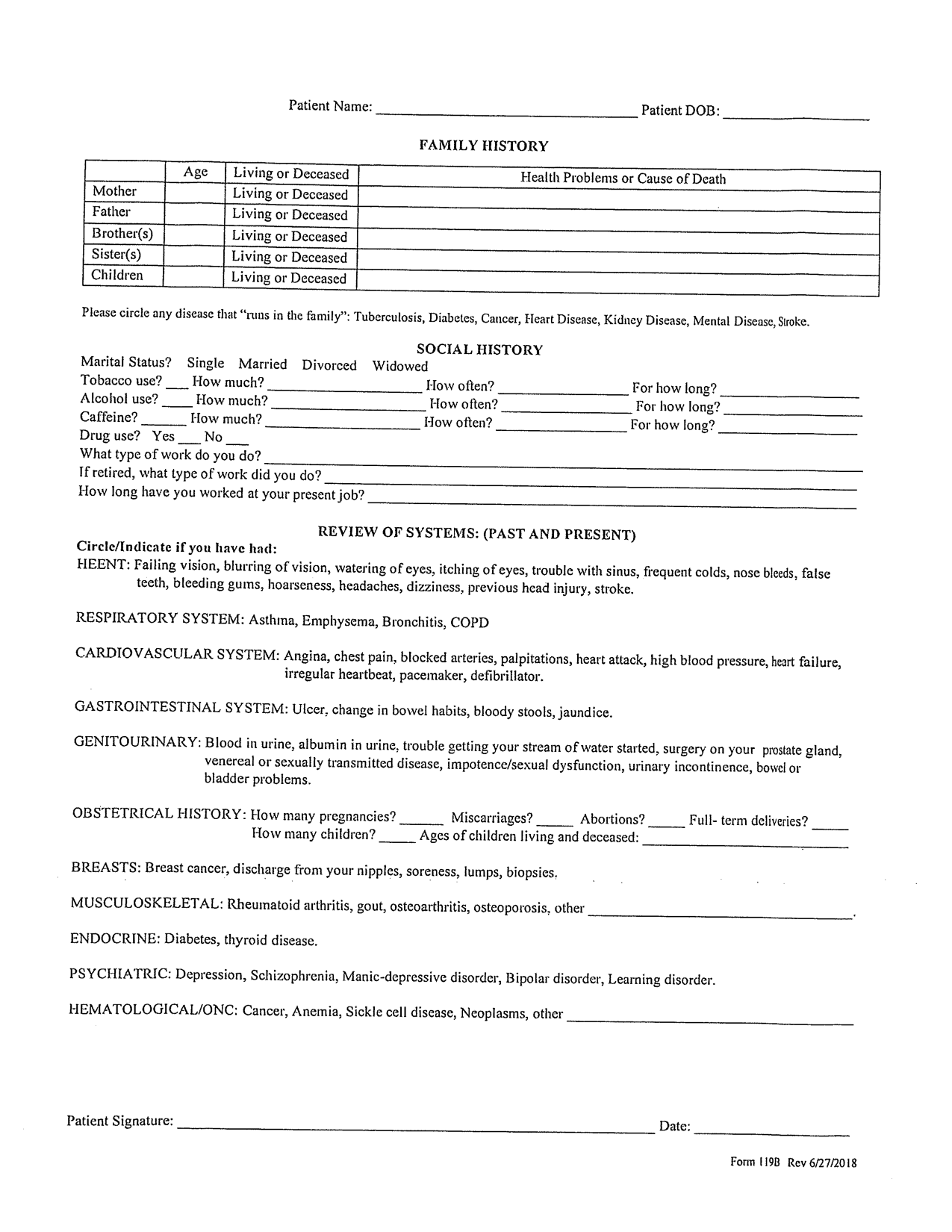
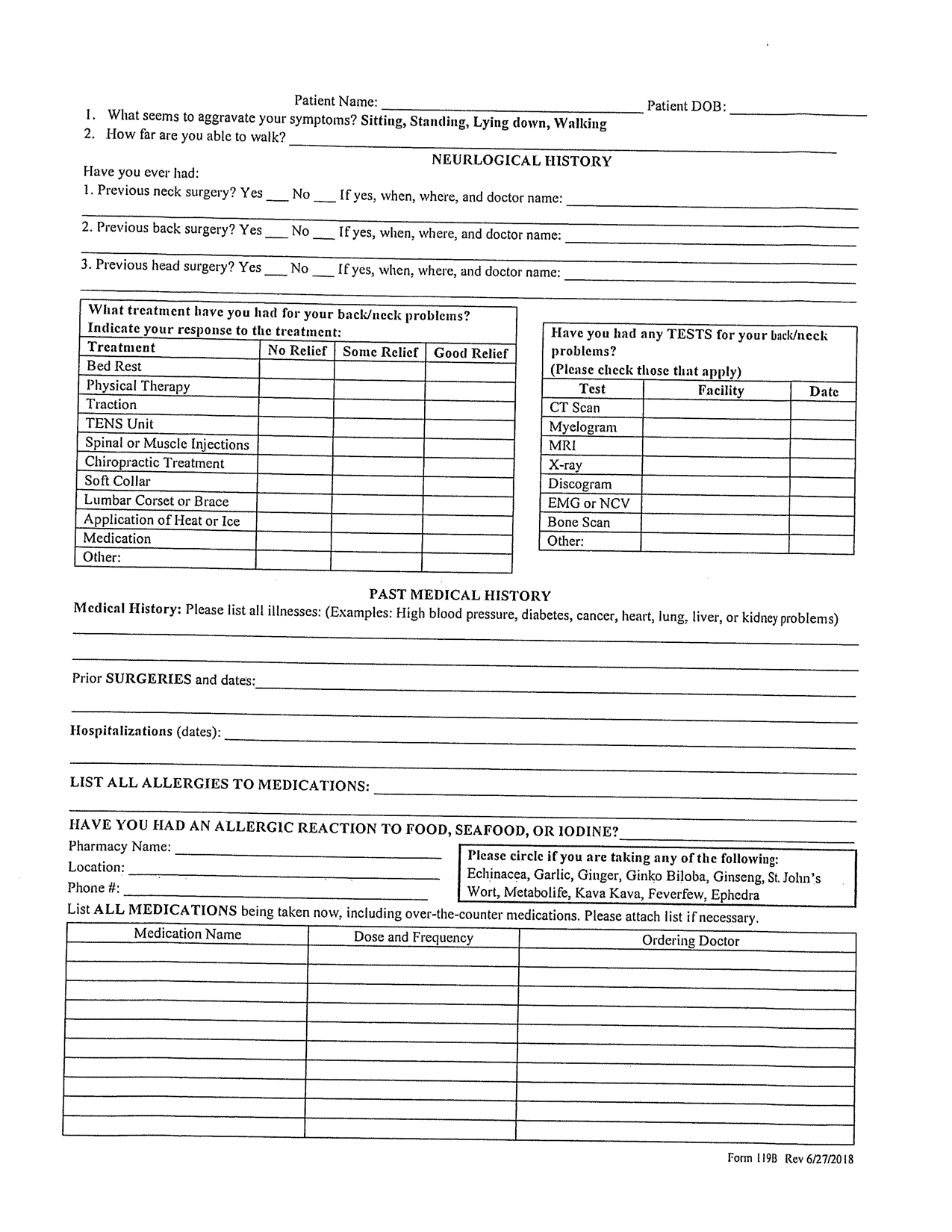
For over 10 years Fort Worth Brain and Spine Institute, a top neurosurgical practice in North Texas, used a system of patient data collection that relied on an physical 8 page form, manual transcription, and copious amounts of time spent manually parsing PHI (protected health information). It was clear that the antiquated system wasted enormous amounts of time and resources as well as created significant security vulnerabilities.
Problem
The legacy system had many interconnected inefficiencies but we quickly realized that the critical problem was the manual processes required to operate the system.
Patient’s were required to arrive to their appointments 45 min early, physically bringing with them all all of their protected health information. After completion of the multi-page form, admin staff were then required to manually populate their internal system before the patient could be seen. Patients often had waits in excess of an 1.5 hours for appointments they had scheduled!
Conclusion: Paper forms and manual processes created operational waste in excess of 90% in certain areas.
Solution
Created end to end encrypted paperless PHI transmission system
-
1
Patient Entry
-
2
Internal System
-
3
Admin Parsing & Distribution
Key Criteria
Paperless Forms
Redesigned entire information system. Entirely digital; intake, transport, and formatted delivery of mission critical data
Admin Data Management
Secure data management tools for medical and administrative uses. Fully HIPAA compliant dashboard and distribution pipelines, ensuring top security of sensitive patient PHI.
Automated Formatting with Custom Templates
Created custom templates and pipelines for insurance and compliance uses. The system automated the processes of patient medical data; parsing, formatting, and distribution to appropriate systems and 3rd parties.
Process
-
1
Adapt and Code Fields
Rewrite questions to be more clear, direct, and elicit the appropriate response.
-
2
Create Digital Form
Intake form redesigned for optimal experience of both patient's and medical staff
-
3
Develop PHI Pipelines
Secure, fully HIPAA compliant pipelines constructed for distribution and delivery of sensitive PHI (protected health information) to appropriate systems and providers.
-
4
Automated Data Packaging
Data sheets packaged and reports generated for appropriate recipients; Service Provider, Medical Staff, Patient
Step 1
Adapt and Code Fields
In order to properly adapt the legacy system, we had to first properly code all of the *necessary* fields into the new format. When coding the questions there were important discretions made on the relevancy of the inputs and eliciting the appropriate response. We ended up redacting or correcting nearly 50% of the total fields in order to more clearly ask for the necessary information.
Through the process of improving the questioning we identified and eliminated significant obscurities. We ran tests with the revised questions implemented within the legacy paper system and the results were significant. Before making any changes to format or structure, the revised questions lowered the rate of unforced user error by 79.2%. Over 90% of patients through a self-reported survey also reported the revised questions as “significantly more understandable”. This data gave us confidence that the intake form contents were complete and concise.
Step 2
Wireframe and Design Digital Form
A mutual understanding was established that a change needed to be made to adapt the manual legacy system into a seamless digital format, but what did this structure actually look like?
Research was done to determine the viability of popular and successful form frameworks taking into consideration the organization’s objectives and criteria.
The legacy paperwork was 8 pages long and over 100 questions, a behemoth of a process that was arduous by its nature of being. We could’ve simply transposed the form into a full-page digital format, but that cramming approach was in part what led to the issues of understandability. Instead I proposed a drastic change in format, one question at a time. I argued that by lowering the cognitive load on patients we could effectively increase both the accuracy and efficiency of completion.
After debate and further research, there was unanimous support for a simple single question response format. Our initial prototype tests resulted in +30% improvements in both efficiency and accuracy of completion.
Single question structure reduces cognitive load improving efficiency and accuracy
Step 3
Develop Form and Architect Secure Pipelines
Due to the sensitive nature of protected health information, it was vital to construct secure pipelines that were in full HIPAA compliance. After data is entered by the patient, the form submits through secure TLS protocol into the centralized organization database without touching any client. The data is then stored in a cloud database that allows authorized administrative staff to access and manage patient data. A rich tool set allows admin staff to filter and sort patient data by field, download specific data for reporting, and correct any errors.
Step 4
Design Data Templates and Automated Data Packaging
In order to efficiently utilizes the patient data in the many contexts that it’s needed, the Ft. Worth Brain and Spine administration needed a dynamic system for and coding and printing data into multiple formats. There are specific reports needed for insurance providers and regulatory reporting which require redundant data formatted in a particular format. We recognized that another key hinderance of the legacy system was the time it took to create reports for each provider. Through a dynamically coded system, I was able to create auto-generated reports for every necessary 3rd party. These reports are simply stored and accessed under the patient and eliminate thousands of hours of yearly wasted labor.
Results
-
↑ Patient Efficiency
Reduced patient’s active completion time over 50% (50% increase in efficiency)
-
↑ Patient Accuracy
Increased patient completion accuracy over 75%.
-
↑ Patient Satisfaction
Over 89% of patient’s reported a “significantly more convenient and pleasant experience”
-
↓ Labor Costs
Eliminated ~$415,000 in annual labor costs. Reduced admin staff workload by over ~40%.
-
↑ Admin Accuracy
Reduced frequency of admin human error from ~100 instances/wk to >10/wk
-
↑ Admin Satisfaction
Over 96% of patient’s reported a “significantly more convenient and pleasant experience”